In the operating theatre, every movement matters. The surgeon executes the steps required to achieve the required clinical objectives and strategically manage the operation, the anaesthetist monitors vital signs, the perfusionist manages life-support equipment, and nursing staff support the other team members and anticipate their needs. To an observer, it might look like perfectly choreographed teamwork. But beneath the surface, something critical often goes unseen. This is the need for shared mental model (SMM). An SMM is a shared mental representation of the actions and communications involved when performing a complex task. The nature and need for shared mental models will be discussed later in this blog.
While surgical teams may excel at their individual roles, thinking as one unified team is an essential requirement. As a result of their training and individual experience, team members will possess an individual mental model of how they operate equipment and interact with other team members. This will include their own mental picture of the procedure, their own understanding of timing, and their own interpretation of what comes next. When these mental models don’t align, miscommunications the likelihood of error will increase, and patient safety can be compromised.
The solution isn’t necessarily more technical training or better communication protocols – it’s ensuring every team member shares a SMM that is appropriate to support interaction needs in a task such as cardiac surgery, requiring the close coordination of several team members.
The development of a SMM for a specific operation is complicated by the fact that surgery teams are formed from pools of the constituent specialists depending upon their availability. This means that the members of team may not have previously worked together and therefore may not possess an SMM which has been optimised for their role in a specific operation. There is therefore a need to develop a process which supports the development of a common SMM for the specialist clinicians in the theatre team. This process also needs field data to be collected so that the SMMs that are developed reflect a consensus regarding what constitutes best practice. This project describes one approach to achieving his objective.
The Hidden Challenge in Surgical Excellence
Cardiac surgery saves thousands of lives each year—but it’s not without risk. Coronary Artery Bypass Grafting (CABG) is one of the most common and complex procedures performed in UK hospitals, requiring seamless coordination between surgeons, anaesthetists, perfusionists, and specialist nurses. Research shows that adverse event rates in cardiac surgery can be four times higher than other surgical procedures, with over 50% of these events being preventable (Gawande et al., 1999). For this reason, the work described in this blog was carried out in a large regional hospital utilising surgical teams for which CABG procedures were the most commonly performed operations.
During critical phases of surgery, each team member focuses on different priorities: the surgeon on the next step, the anaesthesiologist on patient stability, the perfusionist on equipment parameters. Without an effective SMM, situational awareness becomes fragmented and the team’s ability to anticipate and respond collectively is reduced.
This potentially creates cascading problems: team members could struggle to anticipate each other’s needs, critical information could get lost, and when unexpected situations arise, teams may not adapt quickly because they’re not working from the same playbook. The challenge is particularly acute for newer team members, who must master not only their individual role but also learn the unspoken and tacit rhythms of teamwork.
What’s needed is not just better communication – it’s also shared understanding, where every team member operates from the same SMM of the procedure, roles, and timing. Experienced teams develop this informally over time, but this approach can fast-track that process while making tacit knowledge explicit and open to scrutiny.
What Are Shared Mental Models (SMM)?
A Shared Mental Model (SMM) is a common understanding among team members about who’s doing what, when, and why. It’s the invisible framework that allows teams to function as a coordinated unit rather than a collection of individuals. When teams possess accurate SMMs, they can anticipate each other’s needs, communicate efficiently, and adapt quickly when situations change.
Aviation and military operations have long recognised that technical expertise alone isn’t enough. They’ve developed systematic approaches – including pre-flight briefings that rehearse scenarios, expectations, and responses – to ensure every team member shares the same mental picture of the mission.
Medical training traditionally focuses on individual competence, but this doesn’t automatically translate into effective teamwork. The difference between individual expertise and team synchronisation is crucial: when surgical teams develop accurate SMMs, they both think and communicate more effectively.
The Innovation: Video + Task Analysis Training
How do you teach an entire team to think together? The breakthrough combines real surgical video recordings with Hierarchical Task Analysis (HTA) – a systematic mapping technique that breaks down complex procedures, showing what needs to be done, when, by whom, and how tasks interconnect.
Surgical teams collaborate to build detailed HTA maps of their procedures, externalising their collective knowledge about roles and timing. An example of a structure of an HTA map is shown in Figure 1 below.
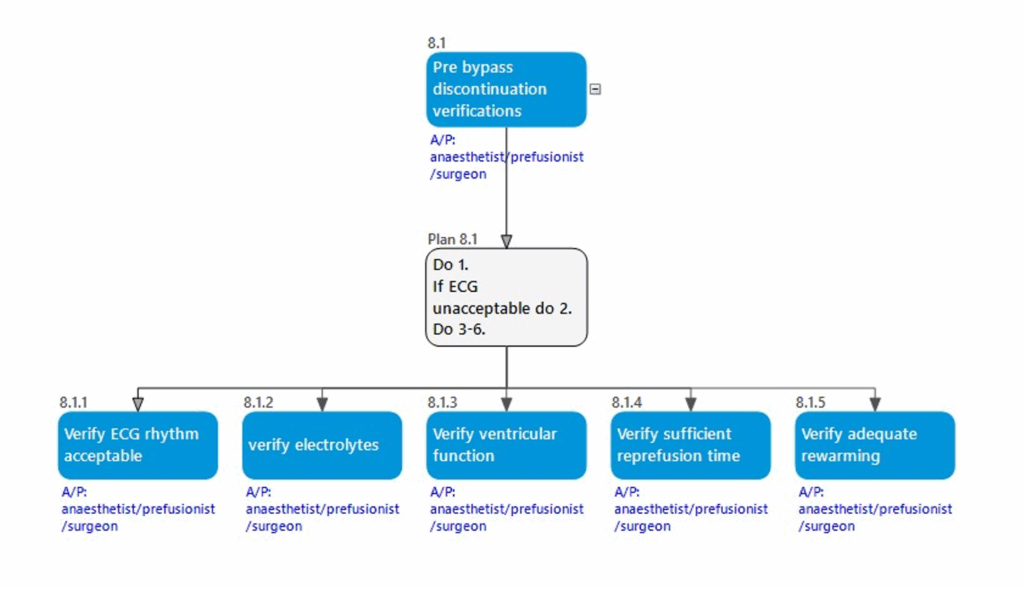
These maps are enhanced with video clips and transcripts of real communications, creating an interactive training resource that links the cognitive structure of the procedure with actual communication patterns.
This approach offers clear advantages: new team members quickly grasp both the overall structure and specific communication patterns that enable coordination. The visual maps make complex interdependencies clear, while video clips demonstrate how expert teams sound when working in synchronisation.
Real-World Results
When tested with surgical teams, participants reported significant improvements in understanding procedural flow and team dynamics. Junior team members showed faster comprehension of their roles within the larger framework, while teams developed enhanced situational awareness and more proactive communication.
Most significantly, the methodology strengthened “team monitoring” – the collective ability to detect and correct potential problems before they escalate. When everyone shares the same mental model, deviations become more apparent, and teams respond more quickly to unexpected situations.
Feedback was overwhelmingly positive. Experienced members found the process helped articulate knowledge they’d developed intuitively, while newer members appreciated having a clear framework for understanding complex team dynamics.

Implementation in Practice
The resource requirements are manageable: video recording capabilities, task analysis software, and dedicated training time. The process begins with experienced teams participating in collaborative mapping sessions, facilitated by someone trained in HTA methodology. This is an offline process, which utilises information gathered from operating theatre videos and open ended discussions.
Video recording requires careful attention to technical and ethical considerations, focusing on team communications rather than surgical details to protect patient privacy. The resulting materials can be used repeatedly with different training cohorts, making it a scalable investment.
We think the proposed methodology could work well in simulation environments and would integrate straightforwardly with existing training programmes – complementing rather than replacing technical skill development.
The Future of Surgical Team Training
This methodology offers a scalable solution as healthcare systems grapple with increasing complexity and staff shortages. We can envision surgical departments where team coordination training is as systematic as technical skill development, with applications extending to emergency departments, intensive care units, and other high-stakes environments.
Perhaps most exciting is the potential to transform medical education itself – preparing healthcare professionals not just to excel in their roles, but to excel together. The SMM could be used as a measure of proficiency.
Given the current pressures on NHS resources in training, a particularly interesting application would be to determine the extent to which the intervention could reduce the time for CABG teams to achieve an acceptable level of proficiency.
Key Takeaways
This was a pilot project with a small sample size which showed promising results. An interesting possibility would be to use the trThis was a pilot project with a small sample size which showed promising results. An interesting possibility would be to use the training materials in conjunction with existing simulation training sessions, and to evaluate the extent to which the methodology could produce measurable improvements in performance.
The path to exceptional surgical team performance lies not just in individual excellence, but in developing a level of coordination that allows teams to think and act as one. Shared mental models provide the framework for this coordination, while innovative training approaches using video and task analysis make it possible to develop these capabilities in a systematic and cost-effective manner.
Key benefits include:
- Accelerated learning – New team members integrate faster and more effectively
- Enhanced safety – Improved team monitoring and error detection capabilities
- Greater efficiency – Proactive communication and better anticipation of needs
- Systematic development – Reproducible methods for building team coordination skills
When surgical teams share the same mental model of their work, everyone benefits – the teams themselves, the institutions they serve, and most importantly, the patients whose lives depend on their coordinated excellence.
Find out more
Find out more about our work in healthcare here: https://www.humanreliability.com/sectors/human-factors-in-healthcare/
Critical competences is part of the Human Factors six topic framework: https://www.humanreliability.com/human-factors/the-human-factors-comah-delivery-guide/
Reference
Gawande A, A, Thomas E.J., Zinner M.J., Brennan T. A. (1999). The incidence and nature of surgical adverse events in Colorado and Utah in 1992. Surgery. 126:66–75.